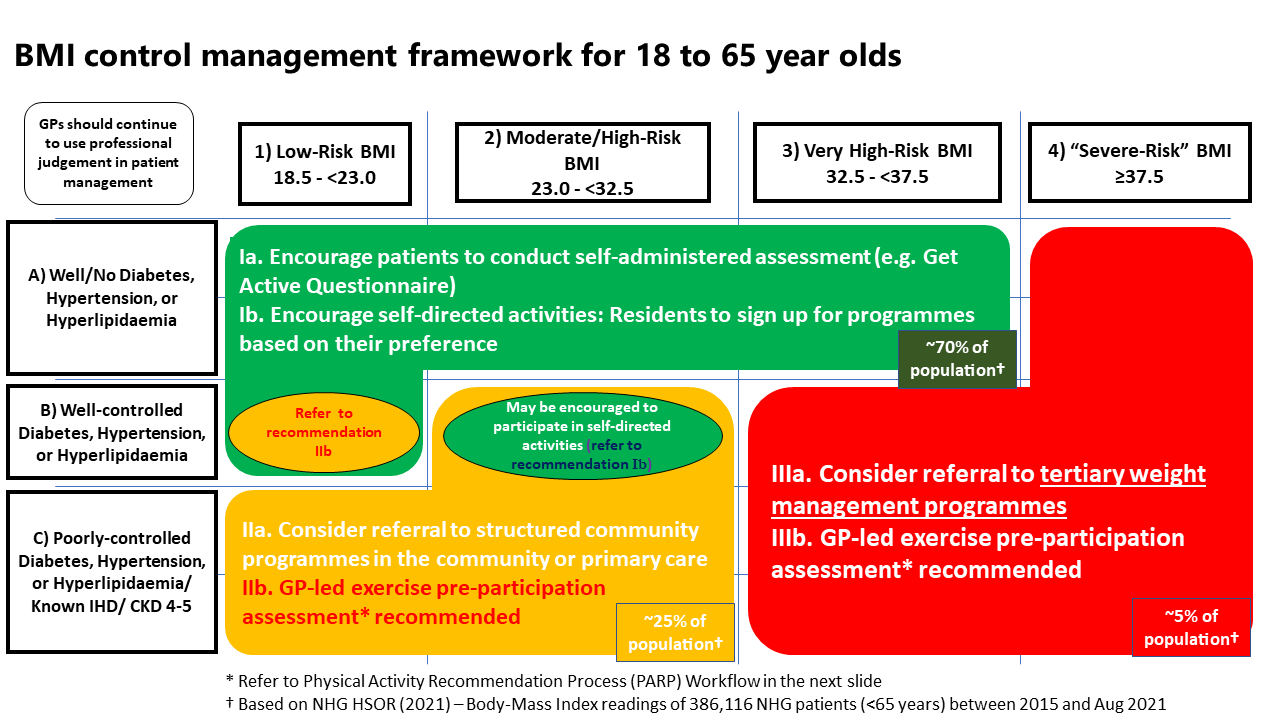
Figure 1 below provides a framework to guide clinicians on the management approach and types of programmes that can be recommended to patients aged 18 to 65, depending on their profile.
For patients above 65 years old, clinicians may examine the history of weight change over patients' lifetimes to gain a more complete understanding of their risk profiles3 (e.g. recent, unintentional weight loss may require further investigation). For patients with high BMI, identify if they have conditions and/or risk factors that would make weight loss desirable (e.g., diabetes, osteoarthritis). For patients with low BMI or who are pre-frail/frail, muscle strengthening activities and multi-component physical activity that emphasises strength and functional balance should be recommended4 to reduce sarcopenia as well as risk of falls and fractures.
Figure 1: BMI control management framework for 18 to 65 year olds.
 Physical Activity Recommendation Process (PARP) Workflow
Physical Activity Recommendation Process (PARP) Workflow
Full list of subsidised weight management programmes offered under Healthier SG
“Green" segment
As patients in this group do not have significant risk factors, you may encourage them to sign up for programmes via
HPB's Healthy 365 (H365) application , including those from HPB, SportSG, People's Association (PA), or healthcare clusters. Refer to list of available programmes . Self-administered assessment may be performed with the recommended tools such as Physical Activity Readiness Questionnaire (PAR-Q) or Get Active Questionnaire (GAQ).
Indicators of physical activity (step count, moderate to vigorous physical activity [MVPA] minutes), patient's diet logging, and participation in national programmes administered by HPB, will be captured on the patient's H365 app.
“Orange" segment
As patients in this group have risk factors that may predispose them to cardiovascular events during physical activity, exercise pre-participation assessment by their enrolled doctor is recommended. Refer to Physical Activity Recommendation Process (PARP) workflow.
Given the need for patient education on exercise, diet and other lifestyle changes for chronic disease management, physicians may consider referring their patients to weight management programmes. Patients with
well-controlled chronic diseases can be referred to structured weight management programmes within Active Health Labs managed by SportSG. Refer to this list of available programmes . You may complete SportSG's referral form for patients who are interested in participating in Active Health programmes.
For patients with
poorly-controlled chronic diseases, the focus of treatment should be the proper management of their chronic diseases. GPs should work with other members of their care teams to achieve this. Concurrently, the care team should counsel patients on diet, exercise and other lifestyle modifications which can contribute to both improved chronic disease and weight management. Patients with poorly controlled chronic diseases should also be monitored more closely by the care team to ensure the safety and adherence to the management regime. Where clinically relevant and beyond the capabilities of the PCN, GPs and/or their PCN teams may seek support for their patients from other available sources (e.g. community / primary care resources, cluster support) for the management of poorly controlled chronic conditions or weight-related issues.
As more patients with chronic conditions are encouraged or prescribed to participate in exercise, other community programme providers (e.g. SportSG) may also refer patients to you should it be deemed necessary to undergo a pre-participation assessment. More details on SportSG’s referral workflow are available here .
“Red" segment
As patients in this group have significant risk factors that will predispose them to cardiovascular events during physical activity, exercise pre-participation assessment by a doctor is recommended. Refer to Physical Activity Recommendation Process (PARP)
workflow .
Given the need for patients to be educated and supported on the interactions between exercise and change in diet on underlying chronic diseases, you may consider referring to specialists or to tertiary-based obesity/ weight management programmes. In general, listed weight management programmes for the “red” segment will accept patients who meet the following criteria:
-
Age:
-
BMI / health status:
-
BMI 32.5 to <37.5 (for patients
with comorbidities) and
-
BMI ≥ 37.5 (for patients
with or without comorbidities)
Some programmes
may also accept patients outside of the stated criteria (e.g., those below BMI of 32.5, or over the age of 65). You may also refer to the list of available programmes for more information on mainstream programmes for weight management.
Once patients transit out of tertiary-based weight management programmes, GPs should consider referring them to community based structured weight management programmes and/or lifestyle counselling. De-escalation of programmes should be performed in tandem with the progress of patients with regard to weight change and chronic conditions patients may have.
* Refer to Resources on Healthier SG Community Partnerships for more information on the types of community-based programmes available in the region, including AHLs and AACs.
Medication1
Medications should not be prescribed for cosmetic reasons and should be used as an adjunct to lifestyle modification. Consider referring to a Specialist for shared care if medications are indicated. Medications licensed for obesity in Singapore include Phentermine, Orlistat and Liraglutide.
Indications for prescribing medications for obesity:
BMI ≥30 kg/m2 with or without obesity-related complications or risk factors OR When BMI is 27.5 – 29.9 kg/m2 among Asians with co-morbidities or complications of obesity such as hypertension, Type 2 diabetes mellitus.
Surgery1
Indications: Clinically severe obesity
For Asians, BMI ≥37.5 kg/m2 OR BMI ≥32.5 kg/m2 with conditions like type 2 DM, hypertension, lipid disorder, fatty liver, polycystic ovarian syndrome, obstructive sleep apnoea and metabolic syndrome.
Consider referring to specialists or to tertiary-based obesity/ weight management programmes should surgery be considered. Depending on the procedure, the mean weight loss after 10 years ranged from 14 to 25%.

